Self-healing and Self-destruction – Part 2
Event data
- Datum
- 4. 4. 2017
- Host
- Mini-Med Studium
- Location
- Van-Swieten-Saal der Medizinischen Universität Wien
- Event-type
- Vortrag
- Participants
- Univ.-Prof. Mag. Dr. Wilfried Ellmeier, Institut für Immunologie, MedUni Wien
- Ao. Univ.-Prof. Dr. Clemens Scheinecker, Universitätsklinik für Innere Medizin III, MedUni Wien/AKH Wien
- Univ.-Prof. DI Dr. Hannes Stockinger, Institut für Hygiene und Angewandte Immunologie, MedUni Wien
This is the second part of the talk on the immune system. Prof. Stockinger was speaking about the possibility of B and T-lymphocytes to produce a much greater antigen receptor variability than that which would be possible by germline determination.
Recombination of gene segments
The secret of recombination was discovered by Susumu Tonegawa (who won the Nobel Prize in medicine in 1987 for this). He was the first to discover that genes can be recombined from gene segments. As such, it is possible, for example, for T-lymphocytes 1 to take V-segment 70 (gene segment – we have 70 V) and J-segment 2 (of which we have 61) and the result is a corresponding antigen receptor (which is, for example, effective against polio). By way of analogy, the B-lymphocytes 2, akin to a random generator, take a segment from V and J and as a result there is a completely different antigen receptor. Through the combination of different gene segments, it is possible for our B and T-lymphocytes to produce around 10,000 different antigen receptors. The gene segments, however, have also to be connected and this (so-called connection diversity) occurs as a result of a random selection of alkali. As such there is an almost infinite possibilty to produce recognition structures (the antigen receptors). For B-lymphocyte 3 it is, for example, possible to take cell 1 V-segment 70 and J-segment 2 but to produce a completely different antigen receptor due to another connection than cell 1.
If a sickness is appraoching …
This would be treated therapeutically, e.g. with antibiotics (this leads to a slowing down of the bacterial growth) and a B-lymphocyte or T-lymphocyte would possibly form a corresponding antigen receptor for this bacterium.
In the case of existing antigen receptors against a bacterium, induction via dendritic cells would lead to a growth of a B-lymphocyte/T-lymphocyte. And now the race begins between the growth of one’s own immune cells and the bacterium. The course is also dependent on the intensity of the infection (in this context: do not forget the significance of washing your hands!).
This is due to the generation time of the B and T-lymphocytes (which amounts to six hours i.e. after six hours they split up after induction). At this rate, there are already one million immune cells on day five, and on day eight, around four billion cells.
Memory cells
During this increase, memory cells are also produced. After the bacterium has been killed, most of the immune cells also have to disappear again as space has to be created.
This is the “predictable immunity” – in the course of life, we adapt to pathogens so that we are protected. These can be read in the framework of the antibody titer. This knowledge is necessary in medicine for the principle of vaccination. Here weakened or parts of pathogens are used in the body to develop memory cells.
Control of the system
For the T-lymphocytes, this occurs in the thymus. The progenitor cell comes from the bone marrow, wanders to the thymus, grows there and begins to express its own antigen receptors. Those cells whose receptors are directed against components produced by the body or against harmless components die (“aptoptosis”). Only 2-3 % of all T-lymphocytes are ultimately able to wander from the thymus into the blood – this is, however, not directed against itself. Dysfunctions include, e.g. auto-immune disorders (here the body’s own tissue is attacked as not one’s own) or cancer (modified tissue is tolerated as one’s own).
How can the body differentiate between dangerous and harmless? It is thought that this occurs in the gastrointestinal tract.
In this field, the personnel at the Medical University in Vienna are global leaders.
If it is known which allergy antigens there are, it is also possible to recognise certain cells with special antigen receptors and to eliminate them therapeutically. There are already excellent therapy programmes which will subsequently be presented by Prof. Scheinecker.
Therapeutic possibilites in the case of auto-immune disorders
Prof. Clemens Scheinecker spoke about the therapuetic possibilities in the case of a pathogenic immune system. As already mentioned, when the body turns against itself, auto-immune disorders result. Paul Ehrlich was one of the first to recognise that the immune system can also make us sick and referred to this disorder as “horror autotoxicus”.
A well-known drug which has been used for a long time in this context is cortisone. This is an endogenic hormone of the adrenal glands which was discovered in 1935 and first used in 1948 with phenomenal success. This is still considered a milestone in pharmacological history. Nevertheless, the side-effects can be very unpleasant, in particular if taken over a longer period of time.
Currently, the strongest known immunosuppressive is cyclophosphamide, which is also used in chemotherapy. This drug can also cause extreme, undesirable side-effects.
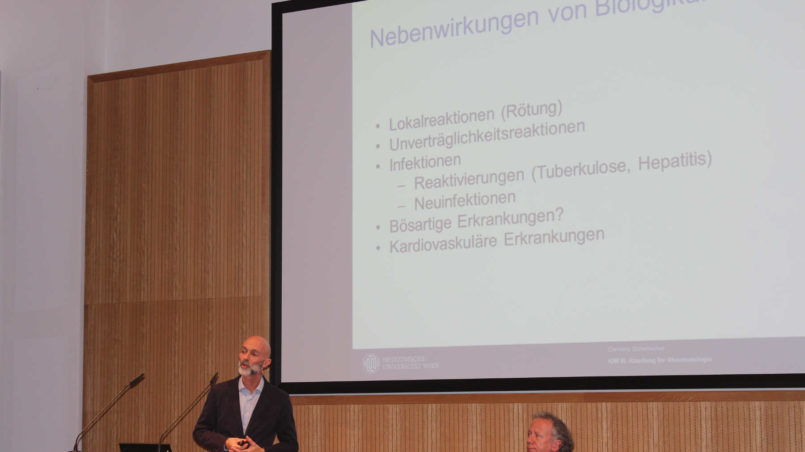
These drugs were developed around 20 years ago – the so-called “biologicals”. These can disable the inflammatory messengers (“cytokines”, see article 1), block the activating of immune cells, eliminate entire populations of cells (e.g. the B-cell population) from the system or block the signal paths within cells.
It is important to stress that these drugs were studied in animal trials in order to subsequently be used in therapy for humans (“from bench to bedside”). Of course the biologicals also have side-effects which, however, are typically not at intensive as those from the older drugs (there are, however, problems in particular in the case of cardiovascular diseases). Among the ten bestselling drugs worldwide, four are biologicals (especially in the rheumatology/hematology field). But the high therapy costs should not be ignored.

This extremely fascinating event was attended by a large audience who also had the opportunity to ask questions. This highlights – despite the complicated nature of the subject – the great significance of and interest in immunology in daily life.